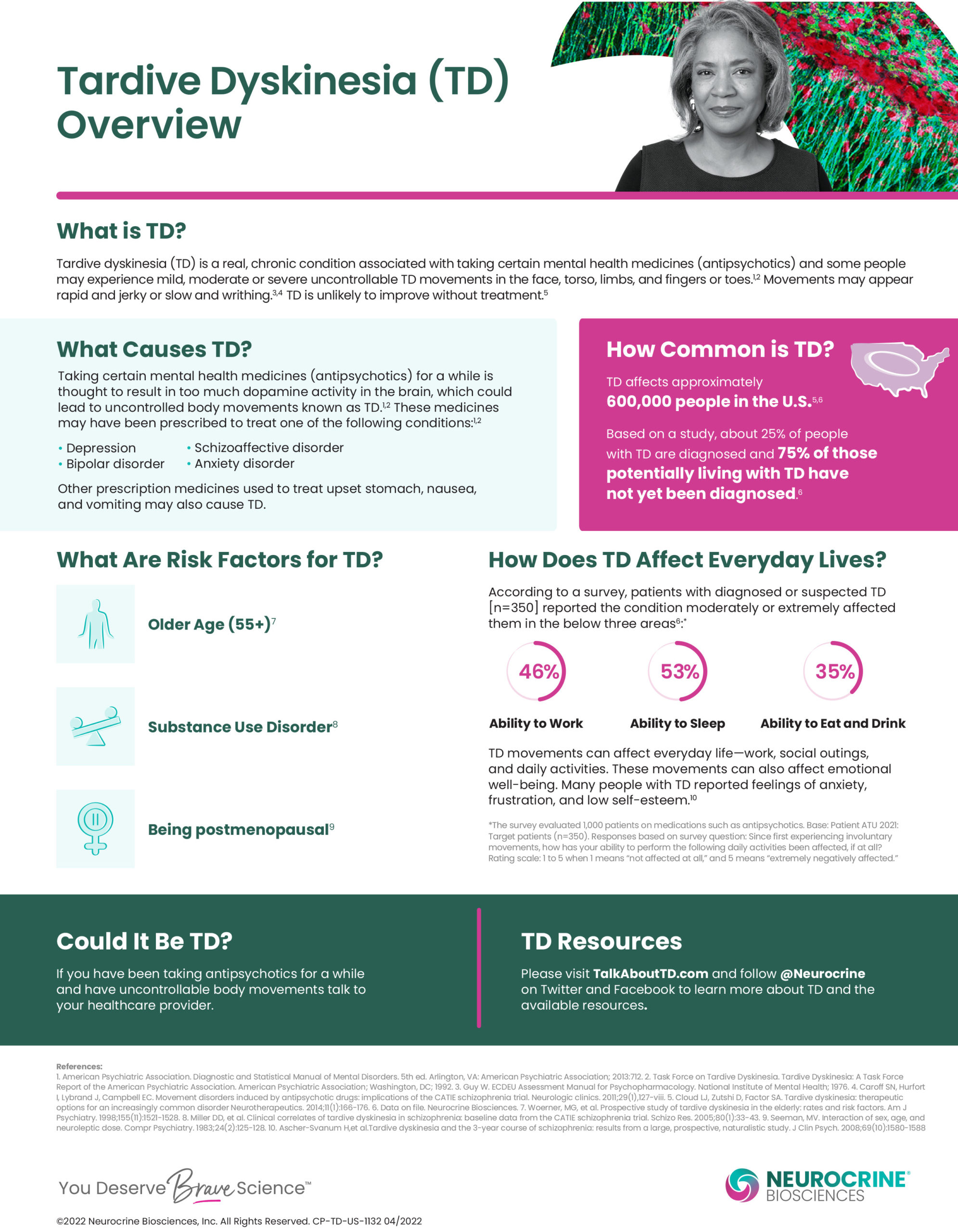
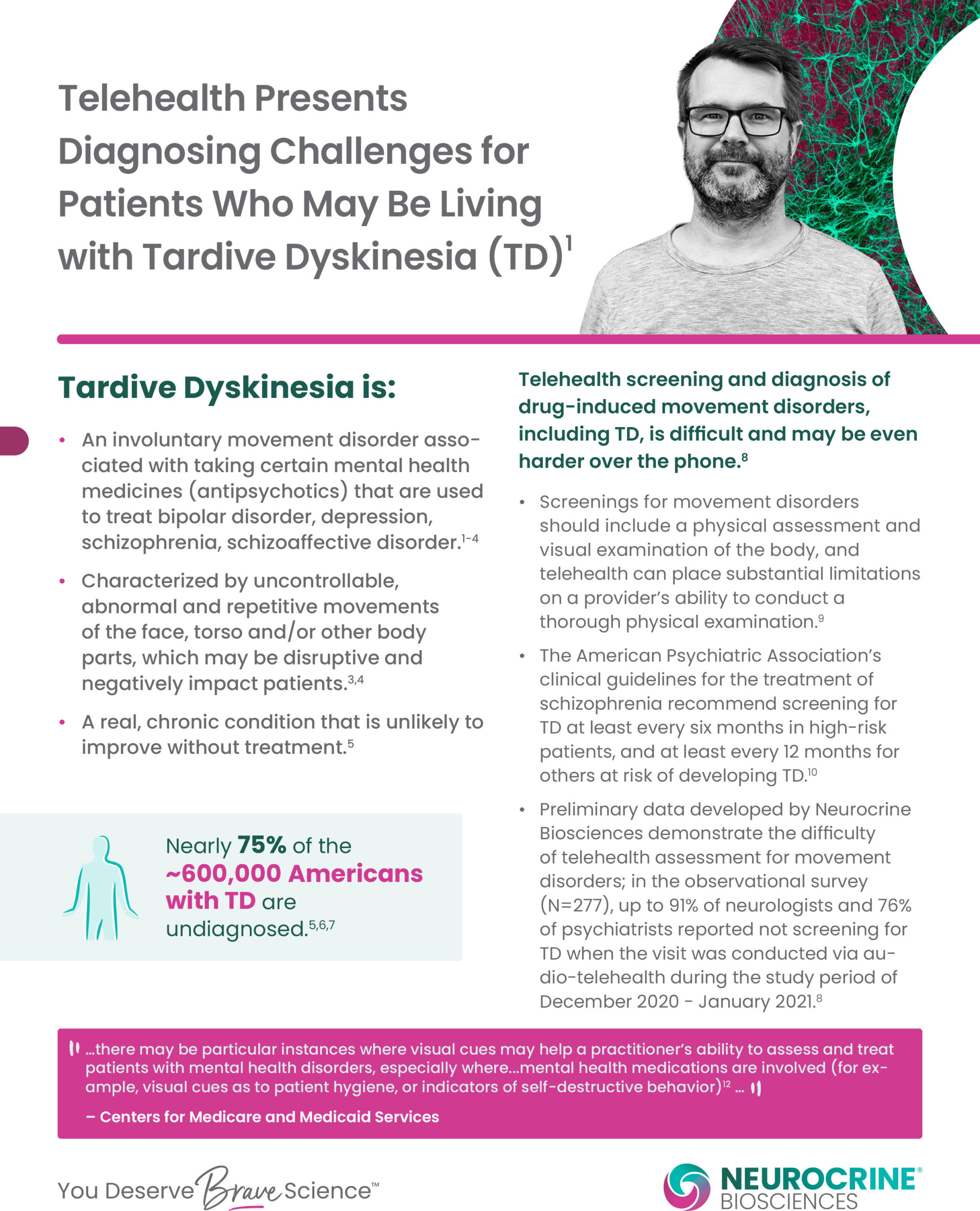
Tardive dyskinesia (TD) is a movement disorder that causes a range of repetitive muscle movements in the face, neck, arms and legs. TD symptoms are beyond a person’s control. These symptoms can make routine physical functioning difficult, significantly affecting quality of life.
Although sometimes associated with conditions such as schizophrenia, TD primarily occurs as a side effect of long-term use of certain medications. It can become a permanent condition even after a person stops taking the medication.
Symptoms of TD can include:
- Jerking hand and leg movements
- Neck twisting
- Difficulty swallowing
- Eye blinking and grimacing
- Lip smacking and involuntary tongue movements
TD symptoms typically occur after several years of taking antipsychotic medications, although they can emerge within just a few months. TD is also related to prolonged use of medications for nausea, and medications that treat neurological disorders, such as Parkinson’s disease.
Anyone taking an antipsychotic may develop TD, but the risk of TD can be higher for certain people:
- Older adults
- Females
- Those with a family history of TD
- Having negative symptoms of schizophrenia
- People of African descent
How Can I Manage The Risk Of Tardive Dyskinesia?
You can help manage the risk by addressing lifestyle factors that increase the potential to develop TD. The risk of developing TD rises with:
- Smoking
- Substance use
- Uncontrolled diabetes
Proactively taking care of your health by quitting smoking, avoiding substance use and managing blood sugar levels can be protective and reduce the risk of symptom onset.
Other steps you can take to help manage the risk include asking your health care provider for routine screening of movement symptoms. Recognizing the symptoms of TD early can help lessen their severity, so these screenings should occur every three months.
You can also ask your provider to review your current medications and discuss options. Although it can still occur, rates of TD appear to be lower with second-generation antipsychotic medications. Long-term use of antipsychotic medication to treat a chronic mental health condition is usually still necessary, but safely adjusting or changing medication may be an effective option.
Examples of antipsychotic medications:
First-generation or older antipsychotics:
- Chlorpromazine (Thorazine)
- Fluphenazine (Prolixin)
- Haloperidol (Haldol)
- Mesoridazine besylate (Serentil)
- Molindone (Moban)
- Perphenazine (Trilafon)
- Pimozide (Orap)
- Thioridazine (Mellaril)
- Trifluoperazine (Stelazine)
Second-generation or newer atypical antipsychotics:
- Aripiprazole (Abilify)
- Clozapine (Clozaril)
- Lurasidone (Latuda)
- Olanzapine (Zyprexa)
- Paliperidone (Invega)
- Metoclopramide (Reglan)
- Risperidone (Risperdal)
- Ziprasidone (Geodon)
It’s important to work with your treatment team to make informed choices about medications and the best way to manage all your health conditions.
How Is Tardive Dyskinesia Treated?
If symptoms of TD develop, your health care provider will evaluate your treatment plan and medication. Your provider may choose to change your medication, or add one specifically designed to improve movement symptoms. It’s important that you don’t abruptly stop taking a medication without talking to your health care provider.
Each person responds to treatment differently, but effective options have emerged over the past several years that help relieve symptoms of TD.
The first level of treatment options include specific movement disorder medications, such as valbenazine and deutetrabenazine. These medications are thought to help by adjusting dopamine reception in areas of the brain responsible for motor control.
Second-level treatment options include clonazepam, which is sometimes given as a short-term medication for muscle rigidity. People have also found relief from the herbal supplement gingko biloba.
For symptoms that are less responsive to these treatments, your clinician may prescribe a drug used to treat movement symptoms in Parkinson’s disease called amantadine. Additionally, there is some evidence that deep brain stimulation (DBS) may be effective when other options have not reduced your symptoms.
Be sure to talk to your provider about potential drug interactions. Of note, a class of medications called anticholinergics have been prescribed in the past with the belief that they improved movement symptoms. However, we now know these medications do not improve symptoms — and may even worsen TD, as well as other cognitive symptoms, particularly when taken with an antipsychotic.
Even mild TD symptoms should be assessed and treated to lessen these symptoms and prevent further impact on daily function and quality of life. If your provider recommends a medication, but you are concerned about its cost, Prescription Assistance Programs (PAP) may be able to help. PAPs can sometimes substantially reduce medication costs.
It is important to work with your prescriber and have honest conversations about your symptoms, treatment and any changes you feel are affecting your health.
Other ways to manage Tardive Dyskinesia
Your health care provider will continue to monitor your symptoms and treatment plan, but you can take an active role in your care by:
- Make sure you have a routine symptom assessment every three months
- Keep track of your symptoms and let your provider know about any new ones
- Talk to your provider about your daily functioning and quality of life
- Practice self-care that includes physical activity
Exercise can help relieve movement symptoms, including tremors and those related to balance, gait and flexibility.12 It also helps balance blood sugar levels and improve hormonal balance for better management of type 2 diabetes.
It’s particularly notable that exercise improves cognitive function and reduces the negative symptoms of schizophrenia and response to chemical signals. These are important factors that affect both the risk for TD and the ability to manage it.
TD can be very troubling, for those who experience it as well as for their families. Although this condition can have a negative impact on quality of life, an informed treatment plan combined with proactive self-care can help effectively manage TD.
Let’s Talk TD: An Overview of Tardive Dyskinesia
NAMI Southwest Washington, Nuerocrine Biosciences along with NAMI Southwest Washington will be hosting “Let’s Talk TD: An Overview of Tardive Dyskinesia” presented by Dawn Vanderhoef, Ph.D., DNP, PMHNP-BC, FAANP Senior Medical Clinical Practice Liaison.
Date: TBD
If you are interested in signing up for future presentations please contact Trisha Charlton of NAMI Southwest Washington directly either via email or phone.
Email: [email protected]
Phone: (360) 695-2823 (101)
Tardive Dyskinesia Fact Sheets
Click images below to enlarge.
A special thank you to Talk About TD for all the information and graphics provided for this webpage.