Welcome to our Crisis System of SW Washington webpage, where you can learn more about the Clark, Klickitat and Skamania County crisis systems in place to help you or someone you love during a behavioral health crisis.
What defines a Behavioral Health Crisis?
A Mental/Behavioral Health Crisis is any situation in which a person’s behavior puts them at risk of hurting themselves or others and/or prevents them from being able to care for themselves or function effectively in the community.
Some examples of a mental health crisis are:
- Threatens to or talks about hurting or killing themselves
- Feels rage or uncontrolled anger
- Increases alcohol or drug use
- Engages in reckless behaviors
- Threatens to harm others
- Feels anxious, agitated, unable to sleep or is having dramatic mood changes
- Sees no reason for living

What to do when you or someone you love is experiencing a Behavioral Health Crisis? Call 988!
In 2020, Congress designated the *new* 988 dialing code specifically to help people experiencing a mental health crises. More than just an easy-to-remember number, 988 is a direct connection to compassionate, accessible care and support for anyone experiencing mental health related distress – whether that is thoughts of suicide, mental health or substance use crisis, or any other kind of emotional distress. This number is now live in Washington State! You can call (multiple languages) or text (English only) with trained professionals to receive assistance. Moving to this easy-to-remember, 3-digit code will provide greater access to life-saving services.
What to expect when you call 988
When people call or text 988, they will be connected to trained call specialists that are part of the existing National Suicide Prevention Lifeline network. These trained call specialists will listen, understand how their problems are affecting them, provide direct support, and connect them to their regional crisis services if necessary to provide local resources or an in person response.
Who will answer?
Phone calls are normally answered within 30 seconds by call Specialists who will gather information and ensure you are connected to the appropriate resource for further crisis intervention.
What happens when you call the crisis line?
The 988 operator will ask you for basic information like name, date of birth, phone number, and reason for the call. If you would like to remain anonymous they will still provide support. Once that is done they will connect you with one of our trained staff or volunteers to discuss the reason for your call, and to help you determine next steps that meet your individual needs.
What if you are calling on behalf of someone else?
The 988 operator will ask for basic information on who you are calling about, including name, date of birth, phone number, and reason for calling. If these pieces of information are unknown they will still work with you to get connected the appropriate resource for whomever you are calling about.
What if you need an in person response?
Crisis Connections will connect you with a Southwest Washington regional crisis line specialist to assist in the dispatch of mobile crisis teams, and in the dispatch of Designated Crisis Responders for Southwest Washington.
Southwest Washington Regional Crisis Line: (800) 626-8137
Is staffed by a trained team of mental health professionals and certified peer counselors. A plan will be developed with you to meet your immediate behavioral health needs.
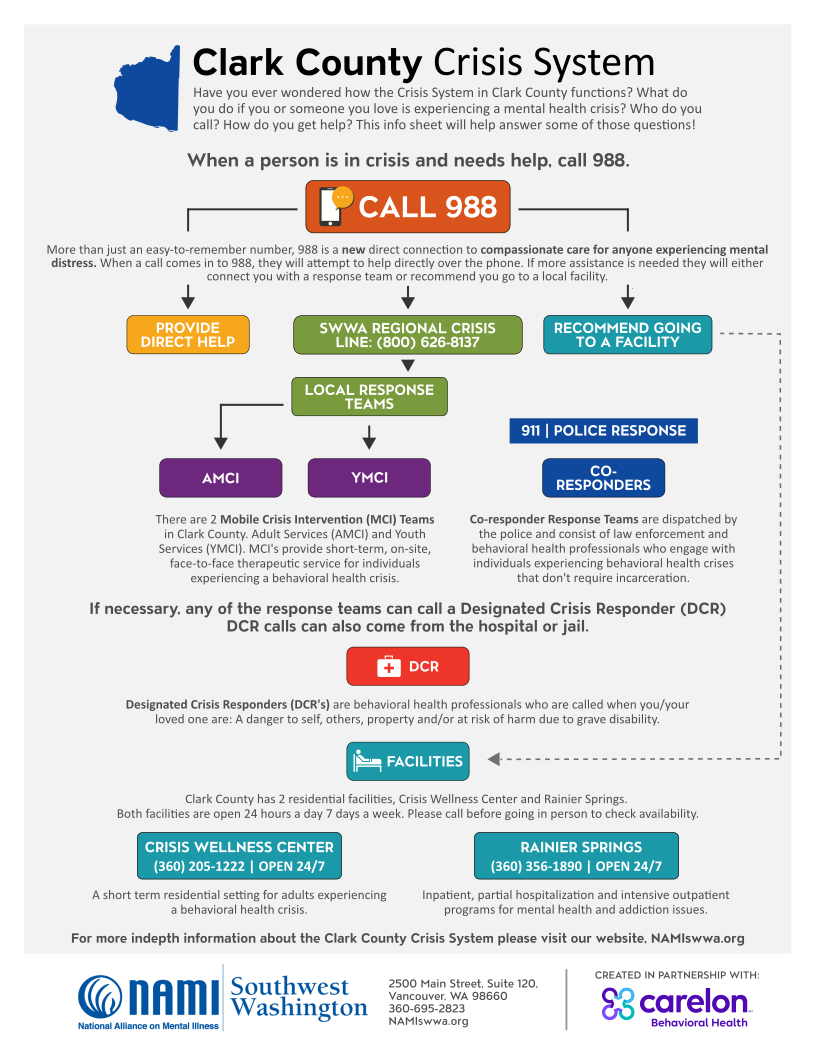
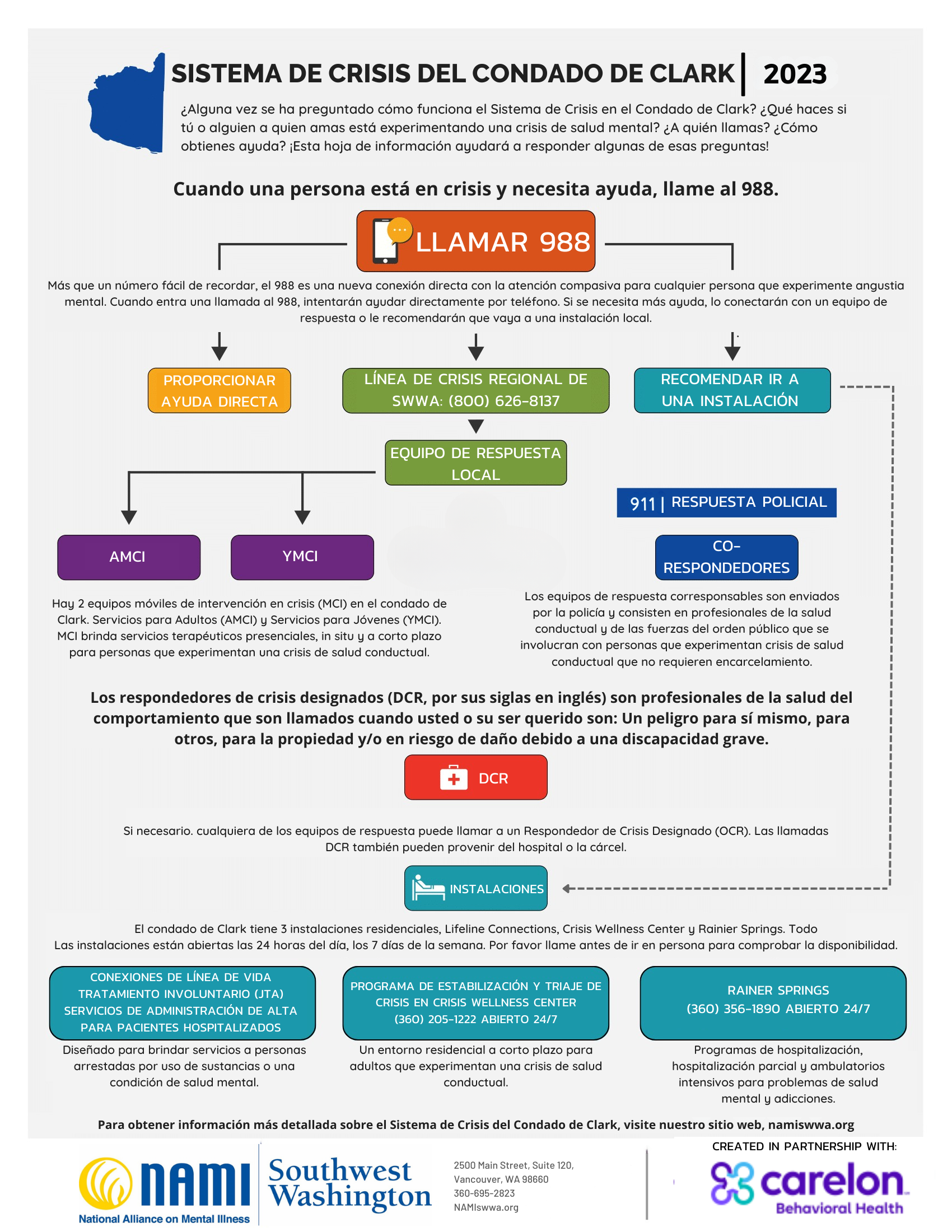
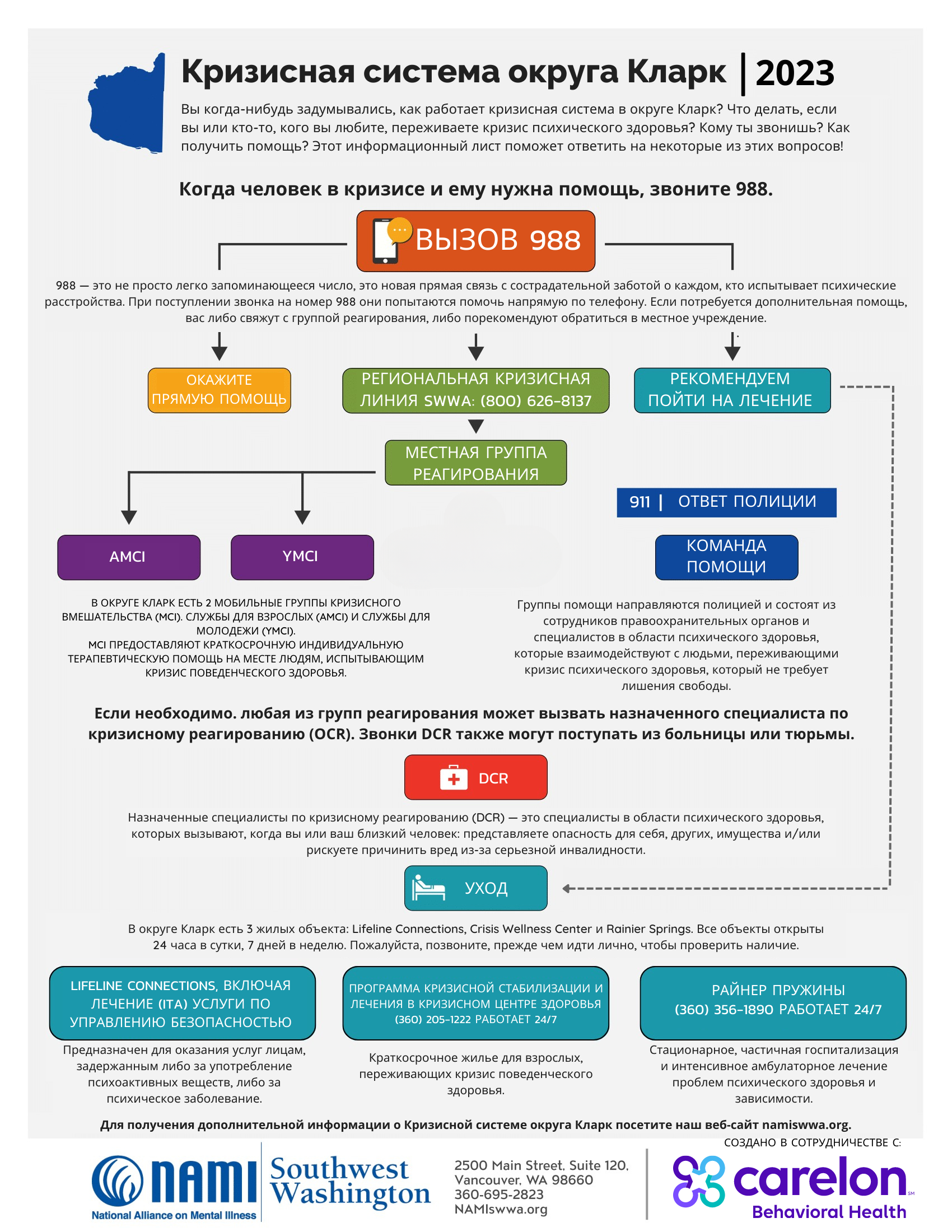
Below is an infographic to help understand how the different pieces of this system function to help those in need in Clark County. Klickitat and Skamania counties have significantly less available in regards to crisis response. What each county offers is listed in the “In Depth Breakdown of our Crisis System” below the graphic.
Please click an image below for a fully downloadable version of this document:
In Depth Breakdown of our Crisis System

The first step when you or someone you care about is experiencing a mental health crisis, is to call or text 988. The trained call specialists will ask you a series of questions to determine what your situation is and how they might help. Their first goal is to help you directly but if necessary they will get you connected to the regional crisis line.

[CLARK | KLICKITAT | SKAMANIA]
The regional crisis line call specialist will assist in dispatching a Local Response Team or will recommend you seek help at a Local Facility.

There are 2 Mobile Crisis Intervention (MCI) Teams which make up the local crisis response in Clark County. Adult Mobile Crisis Intervention Services (AMCI) and Youth Mobile Crisis Intervention Services (YMCI). MCI’s provide short-term, on-site, face-to-face therapeutic service for individuals experiencing a behavioral health crisis.


[CLARK ONLY]
AMCI and YMCI offer crisis assessments and will engage in a crisis planning process, up to 7 days of crisis intervention and stabilization services including: on-site face-to-face therapeutic response, psychiatric consultation and urgent psychopharmacology intervention, as needed, and referrals and linkages to all medically necessary behavioral health services and supports, including access to appropriate services along the behavioral health continuum of care.
Adult MCI (AMCI) teams serve individuals over 18+ and consist of a mental health professional and a peer team. AMCI teams respond within 90 minutes (average of 50 minutes), in person from 8am-12 am, 7 days a week.
Expectations: No guns/weapons or a specific safety plan is in place around restriction/removal of guns. Dogs and other animals are put up, and if applicable COVID protocols will be noted before arrival. If risk/safety issues are indicated, AMCI will attempt to co-respond with law enforcement.
Youth (YMCI) teams serves children and youth under 18 and consists of Master’s and Bachelor’s level clinicians, care coordinators, and peers. YMCI teams respond within 90 minutes, in person from 9am-11pm, 7 days a week, 365 days/year.
Expectations: Before a team is sent out, our dispatcher screens for safety within the crisis area. An adult caregiver is expected to be present before we can safety plan.

[CLARK | KLICKITAT]
Co-responder Teams (CRT’s) are dispatched by the police and engage with individuals experiencing behavioral health crises that don’t require incarceration. They provide in person crisis services, 15 minute law enforcement crisis co-response with team of mental health providers and peers. CRT’s provide risk assessment, safety planning, and connection to resources. The only path to a Co-responder is through 911 or the local police, they are not connected with 988, but are still a part of our local crisis response.
Co-responder Teams serves individuals over the age of 18 experiencing a behavioral health crisis who call 911 or come in through a police request. Co-responder Teams consist of a law enforcement officer (LE), a mental health professional (MHP) and a peer team. The CRT’s goal is to be on-site w/in 15 minutes, 8am-12 am; Monday through Friday.
Expectations: Law enforcement officer is on-scene for co-response with mental health professional and peer, or has previously cleared the scene for safety. If no LE present, no guns/weapons or specific safety plan around restriction/removal of guns, and dogs/animals put up.
If necessary, any of the response teams can call a Designated Crisis Responder (DCR). DCR calls can also come from the hospital or jail.

[CLARK | KLICKITAT | SKAMANIA]
Designated Crisis Responders (DCR’s) are behavioral health professionals who are called when you/your loved one are: A danger to self, others, property and/or at risk of harm due to grave disability. Grave Disability refers to a condition in which a person, as a result of a behavioral health challenge, is unable to provide for their basic personal needs. The DCR’s complete Involuntary Treatment Act Evaluations.
Designated Crisis Responders serve children, youth and adults who are experiencing a mental health emergency. The DCR team timelines depend on the setting and staffing but once a Involuntary Commitment (ITA) referral is accepted a DCR attempts to respond within 2 hours (after the individual has been medically cleared) in person 24 hours a day, 7 days a week, 365 days a year.
Expectations: No guns/weapons or specific safety plan around restriction/removal of guns, dogs/animals put up, and if applicable COVID protocols will be noted before arrival. If risk/safety issues are indicated, DCR will attempt to co-respond with law enforcement.

[CLARK ONLY]
Clark County has 3 residential facilities, Lifeline Connections, Crisis Wellness Center, and Rainier Springs. All facilities are open 24 hours a day 7 days a week. Please call before going in person to check availability.

The Crisis Wellness Center offers short term residential setting for adults experiencing a behavioral health crisis. Participants have access to group and one on one therapy, medication management services, and case management services to support with stabilization and successful transition back into the community.
The Crisis Wellness Center serves individuals over the age of 18 experiencing a behavioral health crisis. Upon arrival people are supported by our team of mental health professionals, peer support specialists, substance use disorder professionals, case managers, and medical professionals including psychiatric nurse practitioners. Admissions 24 hours a day, 7 days a week, 365 days a year. Please call before going in person to check availability.
Expectations: People will be screened for COVID 19 symptoms and alcohol intoxication prior to admit. Those that have a BAL over .08 will be referred to another resource such as Lifeline Connections’ Sobering Center. This is a non-smoking facility.
Who can’t they accept? Persons in an acute medical crisis or with chronic medical conditions needing hospitalization. We are able to support individuals with ongoing chronic medical issues. People must be able to self-transfer if in a wheelchair or using another adaptive device. C bags, and injections are fine. We cannot provide any IV support, change ports, or manage acute wound dressings such as someone with significant burns or injuries needing more than basic dressing changes. They also will not accept people who are not able to safety plan, persons presenting with a high likelihood of violence or arson at time of admit and level 3 sex offenders.

Rainer Springs offers inpatient, partial hospitalization and intensive outpatient programs for mental health and addiction.
Rainer Springs serves individuals over the age of 18 experiencing a behavioral health crisis. Admissions 24 hours a day, 7 days a week, 365 days a year.
Expectations: Patients and those who accompany patients are screened for COVID-19 symptoms and we ask you wear a mask per state mandates. We will also provide a full psychosocial assessment and provide recommendations for a level of care that will address the patient’s presenting problems. We also take patients vitals upon arrival, as well as a breathalyzer for those seeking detox services.
Who can’t they accept? Rainer Springs can provide an assessment for anyone, however they also have a list of insurances accepted. We do not accept patients with major medical needs. Please call before going in person to check availability.

Lifeline Connections ITA Inpatient is a DCR (Designated Crisis Responder) referred only based program that places individuals on an involuntary hold. These requests typically come from Emergency Departments, law enforcement, treatment providers, family/friends, and community members.
Lifeline Connections ITA Inpatient Services is a 16-bed program that provides behavioral health services to people detained on a mental health or substance use disorder involuntary hold who pose and imminent risk of harm to themselves or others or grave disability.
Expectations: The length of time someone is detained is determined by the judge in conjunction with the treatment team and is discussed daily. Generally, Initial Detention is 5 business days, Short-Term Commitment is 14 business days, and Long-Term Commitment is 90-180 days.
Who Can’t They Accept? Persons experiencing acute or chronic medical conditions that need hospitalization or have medical equipment that cannot be independently managed. People need to be able to perform ADLs (activities of daily living) such as eating, bathing, toileting. They also need to be able to transfer from bed independently and safely evacuate in the event of a fire. They will not accept individuals who present a high likelihood of violence or arson at the time of admission or who are a level 3 sex offender.
Definitions
Behavioral Health: “Behavioral Health” means mental health and SUD conditions and related services.
Behavioral Health Crisis: A crisis occurs when problems in life are more than you or your loved one’s internal coping skills and external resources can manage.
Behavioral Health Professional (BHP): “Behavioral Health Professional” means a licensed physician, board certified or board eligible in Psychiatry or Child and Adolescent Psychiatry, Addiction Medicine or Addiction Psychiatry, licensed doctoral level psychologist, Psychiatric Advanced Registered Nurse Practitioner (ARNP) or a licensed pharmacist.
Certified Peer Counselor (CPC): “Certified Peer Counselor (CPC)” means Individuals who: have self-identified as a consumer of behavioral health services; have received specialized training provided/contracted by HCA, Division of Behavioral Health and Recovery (DBHR); have passed a written/oral test, which includes both written and oral components of the training; have passed a Washington State background check; have been certified by DBHR; and are a registered Agency Affiliated Counselor with the Department of Health (DOH).
Crisis Services: “Crisis Services (Behavioral Health)” means providing evaluation and short-term treatment and other services to Individuals with an emergent mental health condition or are intoxicated or incapacitated due to substance use and when there is an immediate threat to the Individual’s health or safety.
Emergent Care: “Emergent Care” means services that, if not provided, would likely result in the need for crisis intervention or hospital evaluation due to concerns of potential danger to self, others, or grave disability according to RCW 71.05.153.
Mental Health Professional (MHP): A psychiatrist, psychologist, psychiatric nurse, psychiatric nurse practitioner, physician assistant supervised by a psychiatrist, or social worker as defined in RCW 71.05.020; A person with a master’s degree or further advanced degree in counseling or one of the social sciences from an accredited college or university. Such persons shall have, in addition, at least two (2) years of experience in direct treatment of persons with mental illness or emotional disturbance, such experience gained under the supervision of a Mental Health Professional; A person who meets the waiver criteria of RCW 71.24.260, which was granted before 1986; A person who is licensed by DOH as a mental health counselor, mental health counselor associate, marriage and family therapist, or marriage and family therapist associate; A person who has an approved exception to perform the duties of a Mental Health Professional; or A person who has been granted a time-limited waiver of the minimum requirements of a Mental Health Professional.
Peer Support Services: “Peer Support Services” means behavioral health services provided by Certified Peer Counselors. This service provides scheduled activities that promote socialization, recovery, self-advocacy, development of natural supports, and maintenance of community living skills. Individuals actively participate in decision-making and the operation of the programmatic supports
Substance Use Disorder (SUD): “Substance Use Disorder (SUD)” means a problematic pattern of use of alcohol and/or drugs that causes a clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school or home.
A huge thanks to Carelon Behavioral Health for partnering with NAMI Southwest Washington to build out this webpage!