By Katherine Ponte, JD, MBA, CPRP
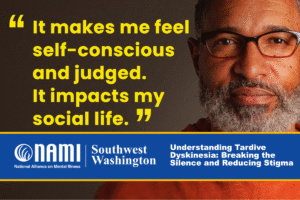
As mental health experts and people living with mental illness know all too well, the stigma surrounding mental illness can be highly destructive. Indeed, negative and discriminatory attitudes that are commonly held about people living with mental illness can adversely impact nearly every aspect of their lives.
Notably, this cultural taboo discourages many people from seeking help. Leaving symptoms untreated often makes them worse — ultimately powering a vicious cycle of stigma and poor mental health. Thus, the impact of stigma can be as severe as the consequences of the illness itself. I know. I live with serious mental illness (SMI) and the forces of stigma.
Addressing stigma is not easy, as these tightly held misconceptions of mental illness are pervasive and systemic. We need much more than time-limited, attention-grabbing sound bite campaigns. We need campaigns of substance. Anti-stigma interventions must seek to do what’s best for people living with mental illness, first and foremost. We need to prioritize approaches that create opportunities for maximum impact and positive outcomes.
Here are several methods and best practices to consider when combatting stigma surrounding mental illness.
Effective Approaches For Reducing Stigma
Research suggests that there are three primary methods that are effective in addressing stigma:
Peaceful protest
This method often targets public incidents of discrimination, including undue use of force against those experiencing a mental health crisis, statements from public figures that perpetuate stereotypes of mental illness and media that mischaracterizes mental illness, to name a few. For example, in 2020, when protests about conduct of law enforcement swept the nation, several demonstrations highlighted the high rate (25%) at which people with SMI are killed during police encounters.
Education
Sharing knowledge and resources is arguably the most common form of intervention. This method seeks to dispel stereotypes and myths about mental illness by sharing up-to-date research, stories of lived experience and professional perspectives.
Contact
Face-to-face contact with people living with mental illness in recovery can be the most effective strategy. A message delivered by someone with mental illness who can share the specifics of their own experience often elicits more empathy and compassion than by if delivered by someone without this experience.
Contact by everyday people can be as effective as contact by public figures, and sometimes more so. Additionally, hearing from people (both those with and without mental illness) who admit to their own stigmatizing behavior and how they came to realize it was wrong can be highly effective. Personal contact has been shown to be effective among many communities, including students, health care providers, first responders and media professionals.
Important Groups To Consider
Based on my own lived experience, here are a few important groups to keep in mind when reducing stigma. Note that stigma interventions should be tailored to the individuals, populations and specific circumstances being targeted.
People with Mental Illness
Self-stigma is pervasive and a major barrier toward recovery. To best target those dealing with self-stigma, interventions should raise awareness about the possibility of recovery. This involves sharing stories of success and encouraging people to pursue recovery by including seeking, accepting, engaging and adhering to treatment and participating in life activities. It is also important for targeted campaigns to be relatable.
Anti-stigma messages targeted to people with mental illness can include:
-No matter how hard or how long you’ve struggled, recovery is possible.
-You can live a full life — thrive, work, have great relationships — even if you have a mental illness.
-Stigma is ignorance, ignore it, don’t internalize it.
Clinicians
Ultimately, I found that stigma from health care providers can be the most harmful. Indeed, I could have reached recovery sooner if I had more constructive relationship with my mental health professionals. Their stigmatizing language and behavior — like the time my former psychiatrist told me that my condition would only get worse — were impediments to healing. As a result, I developed a “why bother?” attitude, as many patients do. A prognosis should be realistic, but it should also be hopeful, no matter how challenging a situation is. For me, and many other patients, coping with the long-term impacts of practitioners’ missteps was critical in reaching recovery.
Anti-stigma messages aimed at clinicians can include:
-You need to provide hope for your patients.
-Patients are often battling internalized stigma, and they need to know that you don’t hold these biases as well.
-Listen to your patients; they know best what will be motivational and helpful when working toward recovery.
Loved Ones and Friends
Stigma coming from loved ones can be the most hurtful, even if it’s unintentional. When our loved ones appear to be ashamed and embarrassed of us, it can be extremely hurtful. For example, my parents and spouse worried about what people might think of them personally and professionally if they learned of my illness. I lost my best “friend” of over 20 years and many more when I got sick, because they did not want to “associate” themselves with someone with a mental illness.
Anti-stigma messages targeted to loved ones can include:
-Loved ones don’t stigmatize loved ones.
-Friends don’t abandon their friends when they get sick.
-Mental illness is not your loved one’s fault.
Becoming A Stigma-Buster
All interventions should be inspired and informed by those of us with mental illness. Accordingly, anti-stigma campaigns should be thoughtfully designed, implemented and executed with our direct involvement. They should always be creative and engaging to maximize reach and adoption — and, critically, they should meet people “where they’re at.” This means that messages should be accessible, while remaining well-informed by reliable evidence-based sources of information and involving individuals with subject matter expertise (such as medical, academic, legal and lived experience).
It’s also important to note that a wide variety of types of interventions can be effective, if well executed. For example, short-term interventions, like NAMI Walks, can be very effective at bringing large groups of people together and create heightened awareness of issues. Meanwhile, long-term interventions, like lobbying government bodies, can lead to meaningful impacts, such as criminal justice reform and legislative change.
These interventions must recognize the realities and possibilities of our lives and, most importantly, they should acknowledge that such possibilities include recovery and full life. A recovery-centric, anti-stigma campaign may be the solution to dismantling stigma while inspiring hope. Ultimately, successful initiatives will always reflect the philosophy of “nothing about us without us.”
Helpful resource: Patrick Corrigan, The Stigma Effect: Unintended Consequences of Mental Health Campaigns.
A word on NAMI: Since its founding in 1979, NAMI has led many highly successful national and local anti-stigma interventions that have bettered the lives of countless people affected by mental illness. Its initiative, NAMI StigmaFree initiative, is simple — and, sometimes, these can be the most effective. Visit the NAMI website and take the StigmaFree pledge now.
Katherine Ponte is happily living in recovery from severe bipolar I disorder. She’s the Founder of ForLikeMinds’ mental illness peer support community, BipolarThriving: Recovery Coaching and Psych Ward Greeting Cards. Katherine is also a faculty member of the Yale University Program for Recovery and Community Health and has authored ForLikeMinds: Mental Illness Recovery Insights.
Source: https://nami.org/Blogs/NAMI-Blog/April-2022/Developing-Effective-Anti-Stigma-Interventions